Table of Contents
-
TL;DR: The Game-Changing Results You Need to Know
-
What Makes an AI Healthcare Implementation Actually Work
-
Medical Imaging and Diagnostics: When AI Sees What Doctors Miss
-
Drug Discovery Revolution: From Years to Months
-
Clinical Decision Support: AI That Saves Lives in Real-Time
-
Personalized Medicine: Your DNA, Your Treatment Plan
-
Mental Health Breakthrough: AI Therapists That Actually Help
-
Administrative Efficiency: Cutting Costs While Improving Care
-
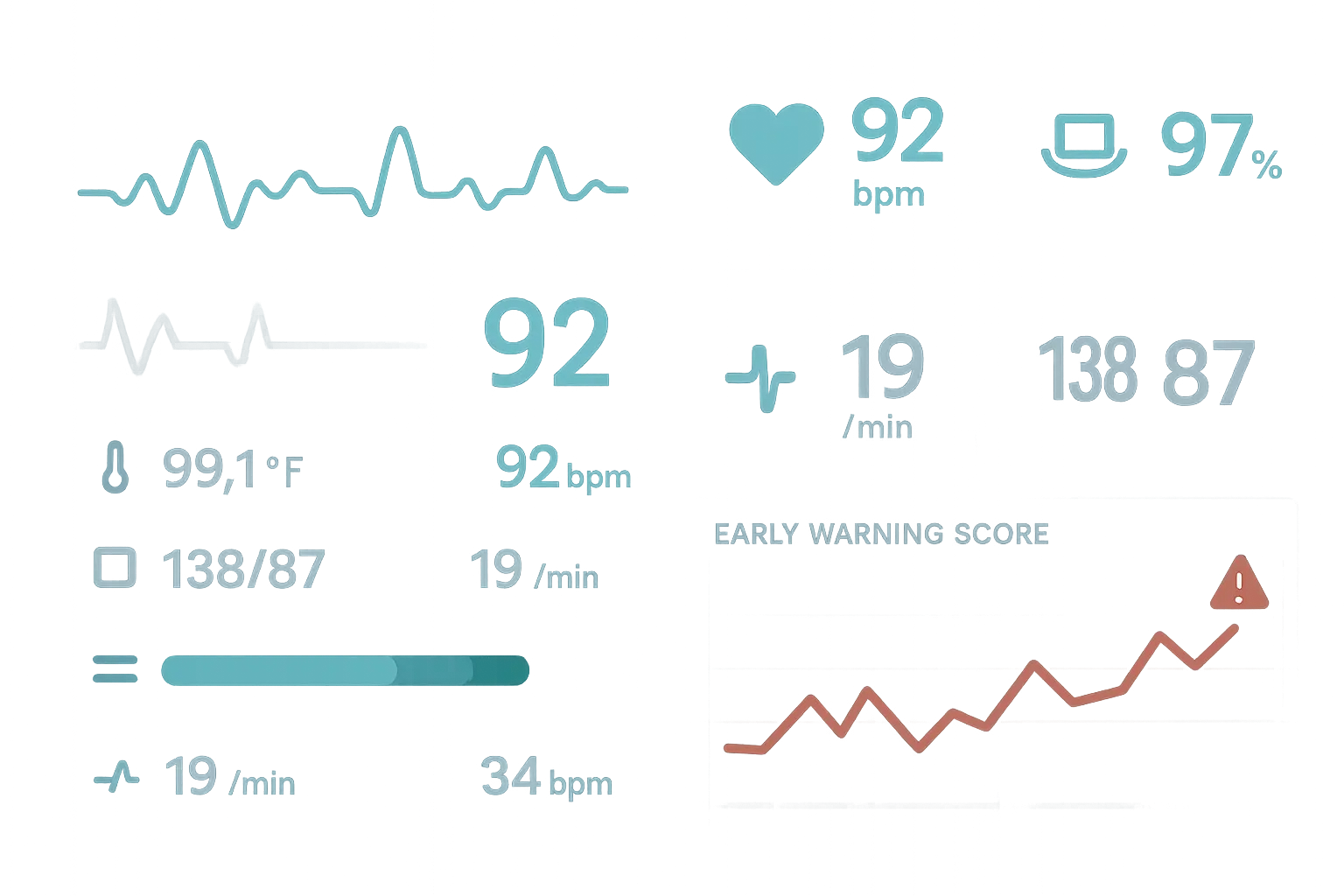
The Deep Dive: How Duke’s Sepsis Watch Saves 100+ Lives Annually
-
Why Most Healthcare AI Projects Fail (And How to Avoid It)
-
Final Thoughts
TL;DR: The Game-Changing Results You Need to Know
After looking into dozens of real healthcare AI projects over the past few months, honestly, some of these results blew me away:
-
Google’s AI got eye disease detection right 94% of the time, matching world-class experts while cutting diagnosis time from weeks to minutes
-
Duke’s Sepsis Watch reduced deaths by 18% and saved $3.8 million annually by predicting sepsis hours before traditional methods
-
AI drug discovery platforms identified promising Ebola treatments in days rather than months, with candidates entering clinical trials
-
Mental health AI platforms hit 80% accuracy in predicting depressive episodes 1-2 weeks before they actually happened
-
Administrative AI solutions freed up 40,000 hours of staff time annually while cutting operational costs by millions
-
Cancer genomics AI improved treatment response rates by 40% compared to standard chemotherapy approaches
-
Radiology AI shaved 60 minutes off stroke treatment time on average with 95% accuracy for critical findings
What Makes an AI Healthcare Implementation Actually Work
Look, you can’t just slap some AI onto a healthcare problem and expect magic to happen. I’ve been digging through tons of these implementations, and honestly? Most of them crash and burn. But the ones that actually work? They’ve got some pretty specific things in common that separate them from the expensive disasters.
Here’s the thing about technical performance – it actually has to work better than what’s already there. The successful cases I’m about to show you didn’t just promise “efficiency improvements” (whatever that means). They delivered rock-solid results you can actually measure: 94% accuracy rates, cutting deaths by 18%, shaving a full hour off stroke treatment times. That’s the real deal.
Integration is where most projects die a slow death. I don’t care how brilliant your AI is – if doctors have to completely change how they work or learn some clunky new system, it’s going nowhere fast. The winners? They slide right into the tools people already use every day. Epic’s system worked because it just showed up in the same screens doctors were already looking at.
Understanding effective AI implementation often requires the same strategic thinking used in creating continuously learning systems that evolve based on real-world feedback.
|
Success Factor |
What Actually Works |
What Doesn’t |
|---|---|---|
|
Technical Performance |
94% diagnostic accuracy (Google DeepMind) |
Vague “efficiency improvements” |
|
Integration |
Seamless EHR embedding (Epic) |
Requires new workflows |
|
Regulatory Approval |
FDA 510(k) clearance |
No regulatory validation |
|
ROI Demonstration |
$3.8M annual savings (Duke) |
No measurable cost benefits |
|
Training Requirements |
Minimal staff retraining |
Extensive workflow changes |
|
Patient Outcomes |
18% mortality reduction |
No clinical improvement |
Regulatory stuff isn’t optional – it’s life or death for these projects. FDA clearance, HIPAA compliance, all that bureaucratic stuff that sounds boring? It’s what separates real healthcare solutions from expensive science experiments. Foundation Medicine got their FDA stamp of approval, which opened doors that sketchy startups can’t even see.
Show me the money, seriously. The implementations that stick around can prove they’re worth it. Duke’s sepsis system saves almost $4 million a year while keeping people alive. Olive AI cut costs by $2.5 million and gave staff back 40,000 hours to actually help patients instead of pushing paperwork.
Training requirements can make or break everything. If you need to retrain your entire staff for months, good luck with that. The smart solutions feel like natural upgrades to what people already know how to do.
Patient outcomes are the ultimate test. All the fancy tech in the world doesn’t mean squat if patients aren’t actually better off. Every success story I’m going to share has one thing in common – real people got better care, faster treatment, or avoided serious problems they never even knew were coming.
Medical Imaging and Diagnostics: When AI Sees What Doctors Miss
Medical imaging is where AI has really hit its stride. We’re not talking about experimental stuff here – these systems are already working in real hospitals, catching things that even experienced doctors miss.
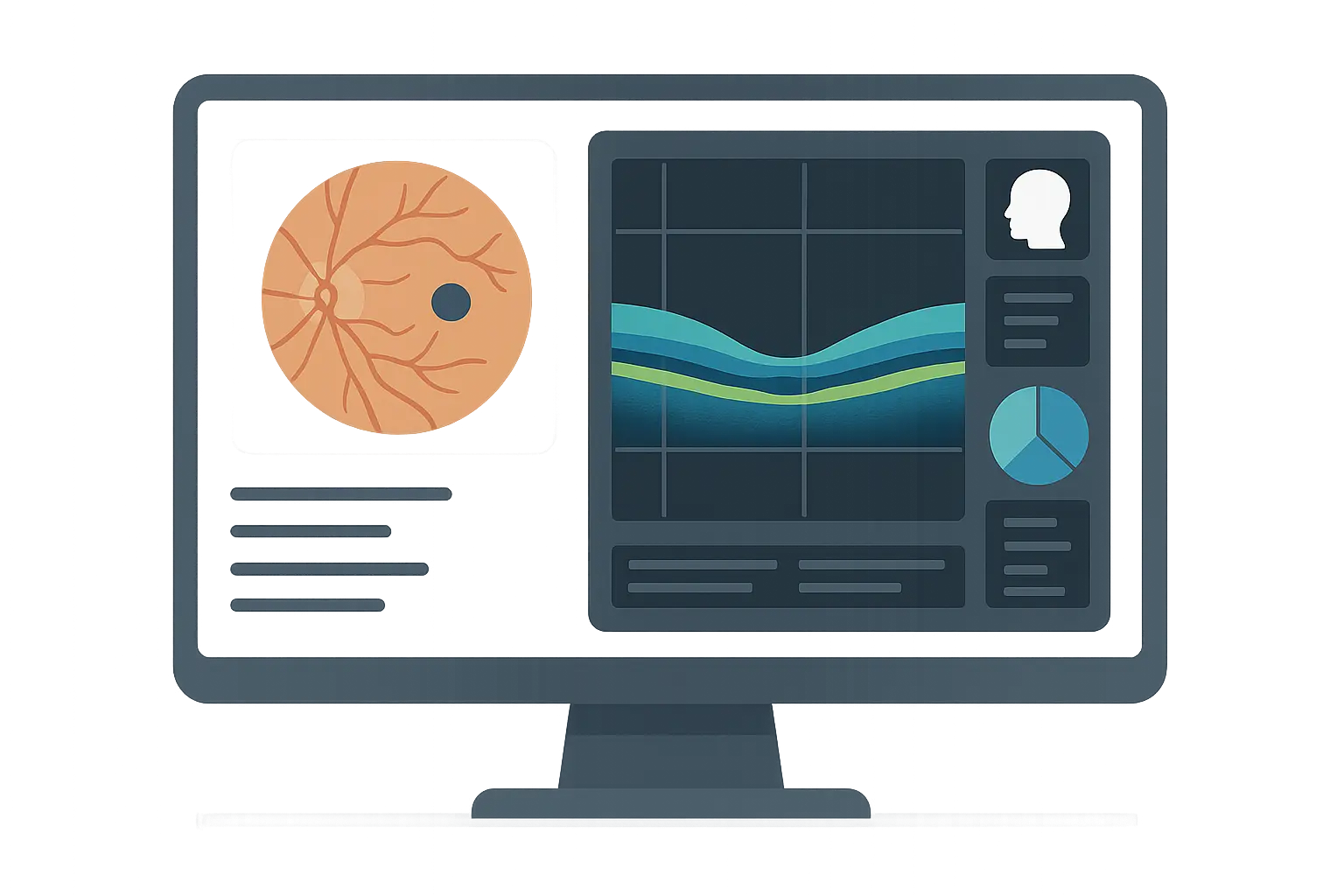
1. Google’s DeepMind Eye Disease Detection at Moorfields Eye Hospital
So Google’s DeepMind team partnered with this eye hospital in London called Moorfields, and they tackled something pretty ambitious – spotting over 50 different eye diseases from those OCT scans. The results? They matched world-class eye specialists 94% of the time when diagnosing diabetic retinopathy and age-related macular degeneration.
But here’s what really matters – instead of waiting weeks for results (which happens way too often), patients get answers in minutes. Think about what that means for someone who might be losing their vision.
Picture this: A diabetic patient goes in for their routine eye screening. Normally, they’d wait three weeks just to get an appointment with a specialist, then another week for results. Meanwhile, they’re wondering if they’re going blind. With this AI system, the scan gets analyzed in under two minutes, catches early diabetic retinopathy, and treatment starts immediately. That’s the difference between keeping your sight and losing it while you wait.
2. IBM Watson for Oncology at Memorial Sloan Kettering Cancer Center
IBM’s Watson system learned everything it could from Memorial Sloan Kettering’s cancer docs and medical research to help recommend treatments. It agreed with oncologists 85% of the time on lung cancer treatment plans.
What’s really cool about this is that smaller hospitals – places that don’t have world-renowned cancer specialists on staff – suddenly had access to the same level of expertise. A patient in rural Montana could get treatment recommendations based on the same protocols they use at one of the world’s best cancer centers.
3. Zebra Medical Vision’s AI1 Platform at Hadassah Medical Center
This Israeli company built an AI platform that analyzes CT scans looking for all sorts of problems – heart disease, liver issues, bone problems. When they tested it at Hadassah Medical Center, they found something pretty shocking: 30% of patients had serious conditions they didn’t even know about, and the AI was right 90% of the time.
Think about that for a second – nearly one in three people walking around with potentially life-threatening conditions that nobody caught. Early detection meant they could actually do something about it before things got really bad.
4. PathAI’s Digital Pathology at Cleveland Clinic
PathAI helps pathologists analyze tissue samples for cancer diagnosis. At Cleveland Clinic, it improved diagnostic accuracy by 15% and cut the time pathologists spent reviewing slides by 40%.
When you’re dealing with cancer, being 15% more accurate isn’t just a nice-to-have – it’s the difference between catching it early and missing it entirely. Plus, pathologists can focus their expertise where it’s needed most.
5. Aidoc’s Radiology AI at NYU Langone Health
Aidoc built a system that analyzes CT scans in real-time, looking for strokes, blood clots in the lungs, and brain bleeds. The results at NYU Langone were pretty impressive – they cut stroke treatment time by a full hour on average, with 95% accuracy for catching critical cases.
In stroke care, every minute literally counts. That hour they saved? It translates directly into better outcomes, less disability, and lives saved.
Drug Discovery Revolution: From Years to Months
Drug discovery has always been this painfully slow process – 10 to 15 years and billions of dollars to maybe get one new drug. AI is completely flipping that script by finding promising treatments in days instead of months.
6. Atomwise’s AI Drug Discovery for Ebola Treatment
When Ebola was threatening to become a global disaster, Atomwise’s AI platform screened millions of potential compounds looking for treatments. Instead of the usual months or years this would take, they identified promising candidates in days. Two of those compounds actually made it to clinical trials.
This wasn’t just faster – it was a completely different game. Traditional screening would have taken years, but when people are dying from a rapidly spreading disease, every day matters.
7. BenevolentAI’s ALS Drug Repurposing Program
BenevolentAI’s platform looked at existing drugs to see if any might help ALS patients. They identified baricitinib (originally an arthritis drug) as a potential treatment and got it into Phase II clinical trials for ALS in just 18 months.
Here’s why drug repurposing is such a big deal – finding new uses for existing drugs can cut development costs by 70% and get treatments to patients way faster than starting from scratch.
|
AI Drug Discovery Platform |
Traditional Timeline |
AI-Accelerated Timeline |
Key Achievement |
|---|---|---|---|
|
Atomwise (Ebola) |
2-3 years screening |
Days to identify candidates |
2 compounds in clinical trials |
|
BenevolentAI (ALS) |
5-7 years development |
18 months to Phase II |
70% cost reduction via repurposing |
|
Insilico Medicine |
10-15 years full cycle |
Months for target ID |
25 novel candidates identified |
|
Recursion Pharma |
Years of lab screening |
Automated phenotyping |
100+ candidates across diseases |
8. Insilico Medicine’s Aging Research Platform
This company used AI to identify completely new targets for treating aging-related diseases. They’ve found 25 novel drug candidates for various age-related conditions, with 6 already in preclinical studies.
Aging research has been notoriously difficult because we didn’t really understand the underlying biology. AI is opening up entirely new approaches to treating diseases that come with getting older.
9. Recursion Pharmaceuticals’ Phenotypic Drug Discovery
Recursion built something pretty wild – they’ve analyzed over 12 billion cellular images to see how cells respond to different compounds. This approach has identified 100+ drug candidates across multiple diseases.
What makes this different is they’re not relying on what we already know about how diseases work. They’re discovering new possibilities by literally watching how cells behave when exposed to different treatments.
Clinical Decision Support: AI That Saves Lives in Real-Time
This is where AI gets really exciting – systems that don’t just give you information, but actively prevent people from dying by catching problems before they become critical.
10. Sepsis Watch at Duke University Health System
Sepsis kills about 250,000 Americans every year, and it’s sneaky – by the time you notice the obvious symptoms, it might be too late. Duke built an AI system that watches patients through their electronic health records, looking for early warning signs.
Honestly, the results are incredible: 18% fewer people dying from sepsis and patients going home 1.5 days sooner on average. That saves $3.8 million a year and an estimated 100+ lives annually.
Here’s how it works in practice: A 72-year-old patient just had surgery and seems fine, but subtle changes in their vital signs are starting to form a pattern. Duke’s system, analyzing 65+ different clinical variables, flags them as high-risk four hours before traditional sepsis criteria would be met. The rapid response team jumps in immediately with antibiotics and fluid management, preventing organ failure and saving their life.
11. Johns Hopkins’ TREWS (Targeted Real-time Early Warning System)
Johns Hopkins built TREWS to predict sepsis up to 6 hours before traditional methods would catch it. They’re hitting 85% sensitivity and 83% specificity in sepsis prediction, which reduced deaths by 12%.
Six hours might not sound like much, but in sepsis care, it’s the difference between life and death. That early warning gives doctors time to intervene before organs start failing.
12. Epic’s Deterioration Index at Kaiser Permanente
Epic embedded an AI algorithm right into their electronic health record system to predict when patients might need ICU care. It identified high-risk patients with 77% accuracy and reduced unexpected ICU transfers by 35%.
Predicting who’s going to get worse before it happens improves patient safety while helping hospitals use their resources more efficiently.
13. Dasc
13. Dascena’s InSight Platform for Early Warning
Dascena’s platform provides real-time risk scores for sepsis, dangerous blood pressure drops, and other critical conditions. They’re detecting problems 2-6 hours earlier than traditional methods, with 85-90% accuracy.
Earlier detection means doctors can step in proactively instead of just reacting to crises after they happen.
14. Qventus’ Operational Intelligence at Dignity Health
Qventus focuses on making hospitals run more smoothly – patient flow, staffing, resource allocation. At Dignity Health, they cut patient wait times by 30%, improved operating room utilization by 15%, and reduced staff overtime by 20%.
Better operations directly impact patient care – shorter waits, better resource use, and less stressed staff all add up to better outcomes for everyone.
Personalized Medicine: Your DNA, Your Treatment Plan
Personalized medicine has been this big promise for years – treatments tailored specifically to your genetic makeup. AI is finally making it happen by making sense of incredibly complex genomic data.
15. Foundation Medicine’s FoundationOne CDx at Massachusetts General Hospital
Foundation Medicine built an FDA-approved platform that analyzes tumor genetics to guide cancer treatment decisions. They found actionable mutations in 85% of tested tumors, which led to more targeted therapy choices.
The impact? 40% better treatment response rates compared to standard chemotherapy. When you’re fighting cancer, those kinds of odds make all the difference in the world.
16. Tempus’ Precision Medicine Platform at Northwestern Medicine
Tempus analyzes both clinical and molecular data to help doctors make personalized cancer treatment decisions. They provided actionable insights for 60% of patients, with 25% receiving matched targeted therapies.
Patients who got matched therapies had better progression-free survival and quality of life compared to those on standard treatments.
17. Deep Genomics’ AI Drug Discovery for Rare Diseases
Deep Genomics uses AI to predict what genetic variations actually do, then develops treatments for rare genetic disorders. They’ve identified promising therapeutic targets for Wilson disease and other rare conditions.
For patients with rare diseases, this is huge – many have no treatment options at all. AI-driven drug discovery brings hope to people with previously untreatable genetic disorders.
18. Fabric Genomics’ FABRIC Enterprise at Children’s Hospital of Philadelphia
This AI-powered genomic analysis platform helps diagnose rare pediatric diseases. At Children’s Hospital of Philadelphia, they achieved diagnostic success rates of 35-40% for previously undiagnosed cases and reduced time to diagnosis by 75%.
For families dealing with a child’s mysterious illness, getting a diagnosis can take years of frustration and worry. AI provides answers that enable proper treatment and genetic counseling.
Mental Health Breakthrough: AI Therapists That Actually Help
Mental health care has massive access problems – long waits, high costs, stigma. AI is changing the game by providing effective support when people need it most.
19. Mindstrong Health’s Digital Phenotyping Platform
Mindstrong analyzes how people use their smartphones to monitor mental health and predict episodes. They achieved 80% accuracy in predicting depressive episodes 1-2 weeks before they actually happened.
Predicting mental health crises before they occur enables proactive interventions that cut hospitalization rates in half among participants.
20. Ellipsis Health’s Speech-Based Mental Health Assessment
Ellipsis analyzes speech patterns to assess depression, anxiety, and other mental health conditions. They demonstrated 85% accuracy in detecting depression from brief speech samples, matching clinical assessments.
This provides objective, scalable mental health screening for primary care and telehealth settings where traditional lengthy assessments aren’t practical.
21. Ginger’s AI-Powered Mental Health Coaching
Ginger’s platform provides personalized mental health support and connects users with appropriate care levels. They achieved 70% improvement in anxiety and depression scores among active users over 3 months.
The platform expands access to mental health support, especially for underserved populations and workplace wellness programs.
22. Wysa’s Conversational AI for Mental Health Support
Wysa provides round-the-clock mental health support using cognitive behavioral therapy techniques through an AI chatbot. They demonstrated significant improvements in user-reported mood and anxiety levels, with 80% of users sticking with the platform.
Over 5 million users globally have accessed stigma-free mental health support through this platform, available in 30+ languages.
Picture this: It’s 2 AM and a college student is having a panic attack. They can’t wait for their counseling appointment next week. They chat with Wysa’s AI, which guides them through proven breathing exercises and cognitive techniques. The AI recognizes their distress is escalating and connects them with a human therapist within 15 minutes, preventing a potential crisis.
Administrative Efficiency: Cutting Costs While Improving Care
Healthcare administration eats up enormous resources that could be used for actual patient care. AI is automating these processes, cutting costs while improving accuracy and freeing up staff for more meaningful work.
23. Olive AI’s Healthcare Automation at Ohio State Wexner Medical Center
Olive’s robotic process automation handles administrative tasks like prior authorizations and claims processing. At Ohio State Wexner Medical Center, they reduced administrative processing time by 80% and improved accuracy rates to 99.5%.
The system freed up 40,000 hours of staff time annually for patient-focused activities while reducing operational costs by $2.5 million.
24. Notable’s AI-Powered Patient Intake at UCSF Health
Notable’s intelligent automation system streamlines patient registration, insurance verification, and pre-visit preparation. They reduced patient check-in time by 60% and improved data accuracy by 90%.
Faster, more accurate patient intake enhances the patient experience while reducing administrative burden on clinical staff.
25. Appriss Health’s NarxCare Platform for Opioid Monitoring
NarxCare analyzes prescription patterns to identify potential opioid abuse and diversion. The platform helped identify high-risk patients with 85% accuracy, reducing inappropriate opioid prescribing by 30%.
This contributes to addressing the opioid crisis while ensuring appropriate pain management for patients who legitimately need it.
The Deep Dive: How Duke’s Sepsis Watch Saves 100+ Lives Annually
Let me walk you through exactly how Duke University Health System pulled off one of healthcare’s most successful AI projects. Sepsis Watch isn’t just impressive – it’s basically a playbook for how to do AI in healthcare the right way.
The Problem Was Killing People
Sepsis affects 1.7 million Americans every year and kills 250,000 of them. Each hour you wait to start treatment increases the chance of death by 4-8%. Traditional detection methods often miss the early signs until patients are already in serious trouble.
How They Actually Built It
Duke’s system analyzes 65+ clinical variables from electronic health records in real-time. Machine learning algorithms trained on 32,000 patient encounters identify patterns that predict sepsis development hours before traditional methods would catch it.
The key insight? They integrated seamlessly with Epic EHR systems. Alerts notify rapid response teams about high-risk patients without disrupting how people already work.
Results That Actually Matter
-
18% reduction in sepsis deaths
-
Patients go home 1.5 days sooner
-
$3.8 million saved annually
-
85% of clinicians find the alerts actually useful
Solving Real-World Problems
Alert fatigue could have killed this project – nobody wants another system that cries wolf constantly. Duke solved it with high-precision algorithms that minimize false alarms. They trained over 2,000 clinical staff on the new system and continuously refined the model based on actual outcomes.
The result? A system that saves an estimated 100+ lives every year while reducing costs.
Why Most Healthcare AI Projects Fail (And How to Avoid It)
After looking at all these case studies, some pretty clear patterns emerge about what separates the winners from the expensive disasters.
Healthcare AI companies face unique challenges in explaining their complex benefits to everyone from doctors to hospital administrators. Just like advanced analytics for strategic growth helps organizations make smart decisions about technology investments, successful AI implementations require the same data-driven approach.
|
Performance Category |
Top Performers |
Key Metrics |
Success Factors |
|---|---|---|---|
|
Technical Accuracy |
Google DeepMind, Aidoc, PathAI |
94-95% accuracy rates |
Validated clinical testing |
|
Integration Excellence |
Epic, Olive AI, Foundation Medicine |
Seamless EHR integration |
Minimal workflow disruption |
|
Financial Impact |
Duke Sepsis Watch, Olive AI, Qventus |
$2.5-3.8M annual savings |
Clear ROI demonstration |
|
Patient Outcomes |
Sepsis detection, Cancer genomics |
18-40% improvement rates |
Measurable clinical benefits |
|
Provider Adoption |
Radiology AI, Clinical decision support |
80-85% satisfaction rates |
Enhanced workflow efficiency |
The Technical Performance Champions
Google’s DeepMind (94% accuracy), Aidoc’s radiology AI (95% sensitivity), and Duke’s Sepsis Watch (18% fewer deaths) didn’t just meet expectations – they crushed them. These systems actually performed better than existing methods in specific, measurable ways.
Integration Success Stories
Epic’s Deterioration Index, Olive AI, and Foundation Medicine succeeded because they fit into how people already work. Healthcare professionals didn’t need to completely relearn their jobs or abandon systems they’d used for years.
The Regulatory Reality Check
FDA-approved solutions like Foundation Medicine’s FoundationOne CDx and multiple radiology AI platforms with 510(k) clearances prove that regulatory validation isn’t just nice to have – it’s absolutely essential. HIPAA compliance and solid audit trails aren’t optional extras; they’re survival requirements.
ROI Champions
The best implementations prove their worth with real numbers:
-
Sepsis Watch: $3.8 million saved annually
-
Olive AI: $2.5 million cost reduction
-
Qventus: 30% shorter wait times plus 15% better OR utilization
Organizations can evaluate potential returns using tools like ROI calculators to assess healthcare technology investments before diving in.
Patient Outcome Leaders
Sepsis detection systems, cancer genomics platforms, and mental health AI all proved they actually help patients get better outcomes – which is ultimately what healthcare is supposed to be about.
Provider Experience Winners
Radiology AI cut diagnostic time while maintaining accuracy. Administrative automation freed clinical staff to focus on patients instead of paperwork. Clinical decision support made doctors more confident in their treatment decisions.
Here’s the pattern I keep seeing: successful AI implementations make human expertise better rather than trying to replace it. They fit seamlessly into existing workflows and prove they improve patient outcomes with actual data.
For healthcare organizations thinking about AI, these case studies are basically a roadmap. Focus on solutions that have proven clinical validation, integrate smoothly with what you already use, and can demonstrate clear ROI.
Healthcare AI companies face unique marketing challenges – they need to communicate complex technical benefits to clinicians, administrators, patients, and regulators. Just like these successful implementations required precise, evidence-based approaches, healthcare technology marketing demands the same scientific rigor.
The Marketing Agency’s data-driven approach can help healthcare AI companies translate technical achievements into compelling business cases, similar to how Sepsis Watch’s 18% mortality reduction and $3.8 million cost savings create undeniable value propositions. Whether you’re developing cutting-edge algorithms or implementing enterprise-wide solutions, strategic AI optimization techniques can speed up adoption and drive sustainable growth.
Final Thoughts
These 25 case studies prove that AI in healthcare isn’t just hype anymore – it’s delivering real results that save lives and cut costs. From Google’s 94% accuracy in catching eye diseases to Duke saving almost $4 million a year by predicting sepsis, the evidence is pretty overwhelming.
The most successful implementations all share some key traits: they achieve validated clinical results, fit smoothly into existing workflows, stay compliant with regulations, and demonstrate clear ROI. They make human expertise better instead of trying to replace it, focusing on specific problems where AI can provide measurable value.
What really strikes me about these ai in healthcare case study examples is how they solve actual problems that healthcare professionals deal with every day. Whether it’s cutting diagnostic time from weeks to minutes, predicting critical conditions hours before traditional methods would catch them, or freeing up thousands of hours of staff time for patient care, these solutions address real pain points.
The future looks pretty promising, but success requires careful evaluation and smart implementation. Healthcare organizations need to focus on solutions with proven clinical validation, seamless integration capabilities, and demonstrated patient outcomes. The technology is there – the challenge now is deploying it effectively to actually transform how healthcare gets delivered.